Nutrition and Digestive Issues
Notes from a talk given by Orla Hynes, Specialist Dietician
Nutrition is often a problem because:
- The anatomical location of the disease can lead to dysphagia [swallowing problems]/delayed gastricemptying/vomiting
- Decreased appetite, weight loss, metabolic alterations & inflammatory state
- Treatments cause additional symptoms which impact on nutrition
- Long treatment pathway – using a combination of chemotherapy, radiotherapy, surgery
Nutrition plays a pivotal role across the entire pathway from diagnosis to survivorship:
- Helps to preserve performance status [ie fitness for treatment]
- Helps to reduce the risk of treatment related toxicities so that you can get full doses of oncological
- Treatments
- Reduce risk of postoperative complications
- Maintain/preserve quality of life
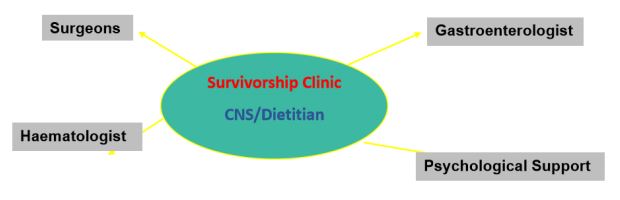
‘Survivorship’:
- Refers to living with or beyond cancer – What happens to the patients after they have finished theirtreatment?
- January 2010 National Cancer Survivorship Initiative published a vision document – findings that NHS are not meeting all cancer survivors’ needs following treatment
- How should we follow up our patients after surgery?
Aim: Quality of Life after Surgery:
Post Surgery:
- Weight loss can be a problem
- Eating and drinking is difficult
- Maintaining a good nutritional status is challenging
- Dietary assessment is important – in determining the problems and strategies to help manage these
- Symptom management
Early Satiety [feeling full] and Reduced Appetite:
- Smaller stomach capacity or none
- Disruption of gut hormones and innervation [vagotomy]
- Need to eat ‘little & often’ and be a ‘grazer not a feaster’
- ‘Hard to change the habits of a lifetime’
- ‘Don’t feel hungry’ is a common complaint
- Worsened by weight loss and malnutrition
- Eating pattern needs to be following a regime, rather than relying on feelings of hunger
Problems with Swallowing:
- Bread and chunks of meat – likely to be a problem
- Sips of fluid with meals can help
- Anastomotic stricture ‘tightening of the [surgical] join’
- Sensation of food sticking
- Range of consistency – Solid foods Soft Diet Pureed Diet/Liquids
- When dietary intake becomes a problem, intervention needs to be considered
- Dietary advice to ensure nutritional adequacy
- Endoscopy +/- stretch
Acid Reflux:
- Common to require antacids
- Loss of gastro-oesophageal junction, new position of stomach or ‘gastric tube’
- Watch out for other signs – cough or hoarse voice in the morning
- Important – can make ‘tightening of the join’ worse
- Dietary advice of limited value as acid reflux is likely – but avoid obvious problematic foods
Bile Reflux:
- Burning, bad taste, nausea
- Delayed gastric emptying
- Responds well to sucralfate suspension
- Endoscopy & stretch
- Delayed Gastric Emptying: Can present as bad reflux
- Appetite in the morning but lessens as the day goes on
- Regurgitation/Vomiting
Management:
- Prokinetics [medication that stimulates the pylorus, bottom end of the stomach, to empty]
- Endoscopy & stretch
Taste Changes:
- Consequence of treatment
- Transient hopefully
- Bile reflux
- Check Vitamin B12 & Zinc
Diarrhoea & Steathorrhea [fatty stools]:
- Decreased gut transit, intestinal hurry
- Loose stools to be expected after surgery
- Improves with time
- Loperamide/Immodium
- Pale floating stools, difficult to flush – caused by fat malabsorption
- Very unpleasant, weight loss, malnutrition
- PERT – Pancreatic Enzyme Replacement Therapy
- Bile Salt malabsorption
- Diagnosed by SeCAT scan
- Cholestyramine/Colesevelam
- Small bowel bacterial overgrowth (SIBO)
- hydrogen breath test
- duodenal aspirates
- antibiotics
- probiotics
- Dietary advice – last resort, fibre, fat, low FODMAPs. Aim to identify and treat cause is priority.
Diarrhoea, Bloating & Flatulence:
- Low FODMAPs diet
- Fermentable Oligo-saccharides Disaccharides Monosaccharides And Polyols
- Last resort…rule out other causes first
- Restrictive and complex, exclusion dietfor 8 weeks, slow and strategic reintroduction of foods. Motivation needed!
- May besuitable in a small number of patients, but not to be implemented without close supervision of a dietitian. Not to betried when on treatment.
Dumping Syndrome:
- Early: bloating/nausea/fullness/palpitations/pain after eating/flushing/sweating/faintness/ loosestools or diarrhoea may follow
- Late: Tiredness/tremor/palpitations/sweating/giddiness
- Complex
- Dietary advice may help
- However seek advice from dietitian – avoid unnecessary restrictions
- ********review other medications************
- Immodium/loperamide
- Acarbose/Octreotide
Fatigue:
- Treatment, stress, anxiety, low mood/depression
- Anaemia – reduced capacity tosend oxygen around the body
- Causes:
- Chemotherapy
- Dietary deficiencies e.g. iron, Vitamin B12, folate
- Iron & Vitamin B12 deficiency is common after surgery
- Regular check of iron, vitamin B12& folate
- Oral iron tablets, IV iron infusion, Vitamin B12 injections
© The Oesophageal Patients Association


